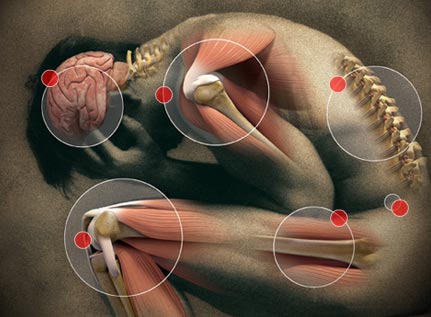
Pain is a personal experience and can’t be experienced by another. We all know what its like to be told to claiming pain, “its not that bad” or worse still, “no it doesn’t”.
It still amazes me that we as healthcare professionals still say this. Pain is definitely associated with poor sleep, but why?
Generally, poor sleep leads to lower pain thresholds and a lower pain threshold decreases sleep efficiency. Obstructive sleep apnea not only disrupts sleep but does so with repeated bursts of stress hormones and a drop in blood oxygen which can be quite significant.
Studies have shown a 55.4% prevalence of chronic widespread pain in patients with obstructive sleep apnea and a greater risk of chronic pain in female than in male patients.
Female patients with obstructive sleep apnea and chronic pain have higher pain and disability levels and a lower quality of life. This seems in general agreement with anecdotal evidence.
So pain and sleep loss may contribute to one another. Experiencing chronic pain can lead to sleep deprivation, but sleep deprivation can also make pain symptoms worse.
It becomes a “chicken and egg” situation where it may be difficult to determine which is causing which – most medical issues have a bi-directional component, simply put, both will influence the other to a degree.
In addition to preventing a person from falling asleep, pain also results in difficulty staying asleep, another reason that OSA and insomnia are linked, both can therefore be chronic.
Research reveals that two out of three people with chronic pain have trouble sleeping.
Chronic pain clinics facilities reported that nearly two-thirds of all adults living with back pain report having trouble sleeping because of discomfort or pains during the night.
While back pain may cause insomnia, other researchers have found that insomnia only makes the symptoms of back pain worse.
Sleep issues are especially common for people with chronic pain, back pain, fibromyalgia or the pain of cancer. In addition, pain is one of the most common causes of insomnia.
Up to two-thirds of patients with chronic pain conditions suffer from sleep disorders of which the most common are insomnia and OSA.
Pain and Sleep Assessments:
Sleep Apnea, as we know, is usually accompanied with co-morbid conditions (related problems) of some type. The ones associated the most are hypertension, obesity, some auto-immune issues such as arthritis other chronic pain and fatigue disorders.
Some of the research findings . Generally, 50% of OSA patients experience chronic pain that is worse than 80-99% of the general population.
Frightening statistics linking OSA with pain.
People with pain experience sleep disturbances that are 80% worse than the general population. 50% of sleep apnea patients experience sleep disturbances worse than 70-95% of the general population.
On average 50% of patients suffer from fatigue that is 90-95% worse than the general public.
Finally, at least 50% of the patients experience fatigue that is no less than 80-99% worse than the general public.
What can we do to break this cycle?
To be proactive in your treatments you should keep a log of your pain. This way when you see your doctor you can create a better understanding for your physician of what’s going on with you.
Charting the following points are helpful:
- When did the pain start?
- How bad is the pain?
- How long does it last?
- Where is it located?
- What does it feel like?
- Is it constant or sporadic?
- Does it come on suddenly?
- Does it get worse or feel better with certain activities?
- How does it limit what you can do?
- Is the pain acute?
- Is the pain chronic which is has a much longer duration and constant?
The more detailed information you can provide the more accurately your healthcare provider can diagnose and treat the issue. Is the pain throbbing, stabbing, aching, burning, tender, cramping, heavy, fearful, tiring or exhausting, and so on.
It seems prudent that careful screening be done for sleep disorders and given the female contingent this must include Upper Airway resistance Syndrome (UARS) which will be discussed in a separate post.
OSA and Fibromyalgia
Because of similar symptoms, patients with fibromyalgia (FMS) should be evaluated for OSA as FMS might occur in patients with OSA. It seems likely that there is a significant association given the relationship of OSA with chronic pain. FMS will be discussed in a separate post.
Irritable bowel syndrom.
IBS (Irritable Bowel Syndrome) – Irritable bowel syndrome (IBS) is assumed as one of the most frequent gastrointestinal disorders, which decreases the patient’s quality of life. IBS pathogenesis, however, is not clearly defined.
It seems that sleep apnea induces or worsens IBS’s clinical symptoms. and studies have indicated evidence consistent with the model of IBS as a disorder of brain-gut interaction.
Overall, studies support a positive association between obstructive sleep apnea and IBS.
Chronic pain syndromes
Chronic pain syndromes – poor sleep lowers pain threshold and pain produce poor sleep. This is an area we will cover in more detail later due to the importance of chronic pain and its effect on lifestyle and the quality of life. Again there is an association.
I get a low grade morning headache
Do you awaken with a “fuzzy head”, sometimes a dull headache at the front. Almost akin to an alcohol hangover. A ‘frontal’ headache – dull and fuzzy, has been linked to inadequate night time oxygenation.
At night, the brain requires 20% of all the oxygen breathed so is both highly active and has requirements for glucose and oxygen.
Awakening headaches are therefore associated withOSA. These headaches are of brief duration, and their occurrence and severity increase with increasing OSA severity.
Treatment of OSA can reduce these headaches. Screening is the first step – ask your healthcare professional.
CLICK BELOW TO RECEIVE YOUR FREE “BETTER SLEEP” GUIDE

Good sleep is crucial to good health and longevity.
Dr. Stephen Bray 2019

